So you’ve been on birth control (BC), perhaps to regulate your cycle, ease menstrual symptoms, or yes, reduce breakouts. For a while things might look fairly stable. Then you decide to stop (or need to stop) the pill, patch, or hormonal IUD — and your skin begins to fight back. This is the story of many women who develop what’s commonly called “post-birth control acne.” I know this can be frustrating, but it’s your body readjusting its rhythms, and your skin is among the first organs to let you know.
The Calm
While you are on BC, especially a combined estrogen-progestin method, several things happen that can reduce acne:
-
The synthetic estrogen increases sex hormone-binding globulin (SHBG), lowering free testosterone and thus reducing sebum (skin oil) production.
-
Ovulation may be suppressed or modified, reducing one source of cyclic hormonal fluctuation.
-
Many dermatologists and gynecologists prescribe BC for acne because of these effects. So from the skin’s perspective: “Hey, things are smoother, oil production less, fewer inflamed breakouts.” For many, that feels like relief.

Image Reference: The Pocket Doctor
The Turning Point: Why Breakouts Come When You Stop
Then you stop the hormonal contraceptive. At first you might breathe a sigh of relief, but then your skin may erupt. Why? This phase can feel like a storm. Key biological shifts:
Androgen Rebound
When you remove the external hormones (particularly estrogen/progestin), your body resumes its natural hormone production. In many women, there’s a surge or rebound of androgens (testosterone or similar) because the suppression is removed. This rise stimulates sebaceous glands more oil, more clogged pores, more acne. One article notes this mechanism both in terms of increased androgen production and increased sebaceous activity after discontinuation of combined hormonal contraceptives. PMC
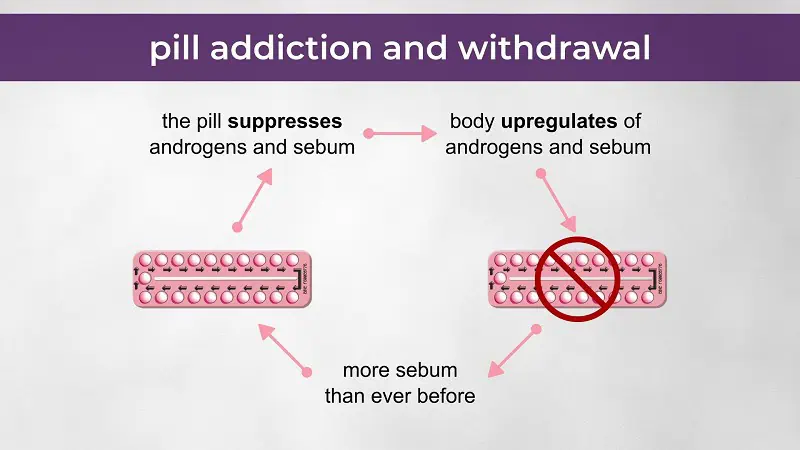
Image Reference: Lara Briden
Hormone Fluctuations & Cycle Restart
Your hypothalamus-pituitary-ovary axis (HPO axis) needs to “turn back on.” Your natural ovulation and hormone rhythm can take a few cycles to re-establish. During this period of instability, estrogen, progesterone, and androgen levels can swing, and your skin often responds to this turbulence with breakouts.
Nutrient Depletion, Gut & Liver Strain
While on BC, studies and clinical observations suggest nutrient stores like zinc, vitamin B12, folate may be reduced; gut microbiome changes may occur; liver processing of synthetic hormones is increased. These shifts may leave you more vulnerable once you stop. For example, if the liver or gut isn't in optimal shape, hormonal metabolites can recirculate, inflammation may increase, and your skin picks up the slack.
Timeline Variability
How long will the rebound last? It depends. Some may rebound in a few weeks, others endure months. One review suggested many women see improvements after 3-5 months if they’re actively supporting health, but for those who aren’t, the struggle can last much longer. Think of it as your skin responding to a transition and transitions take time.
The Personal Reality
You stop birth control because you’re ready to let your body regulate itself again or maybe you’re exploring fertility, wanting a more natural cycle, or simply tired of depending on a prescription to feel balanced. At first, things seem fine. Then, slowly… or sometimes overnight… the breakouts appear. Tender breakouts along the chin and jawline....the kind that feel like they start below the skin before you ever see them. Acne at this stage of life often feels different than teenage breakouts. It can influence:
-
Confidence about walking into work without makeup
-
Social discomfort during conversations
-
Avoidance of photos or mirrors
-
Impact on intimacy, libido, or self-image
And that’s why addressing post-birth control acne isn’t just about clearing skin, it’s about understanding what your body is trying to re-establish hormonally and metabolically. I promise your skin isn’t acting against you. It’s communicating.
A Supportive Plan (No Quick Fixes)
There isn’t a single solution or a one-size protocol, but there are options. And the more you understand what your body needs during this transition, the faster clarity replaces frustration.
Step 1: If You Haven’t Stopped Birth Control Yet: Prepare
If you're planning to transition off hormonal birth control, supporting the body before stopping can make the process smoother. Think of it like setting the prep before a marathon.
Helpful foundations may include:
-
Fiber-rich foods to help the body eliminate hormone metabolites
-
A well-rounded multivitamin with zinc, B12/folate, magnesium, and selenium
-
Stable blood sugar habits — meals with protein, healthy fats, and lower glycemic choices
-
Gut support — a high-quality probiotic, avoiding long gaps between meals, and supporting digestion
This step alone won’t prevent breakouts entirely! It can soften the hormonal rebound effect.
Step 2: After Stopping: Support Hormones
Once you discontinue hormonal birth control, your endocrine system begins to recalibrate. During this time, some women experience higher androgen activity, meaning the hormones that increase oil production may temporarily spike.
Signs of this shift may include:
-
Chin and jawline breakouts
-
Oily skin
-
Irregular cycles
-
Increased body hair or hair thinning at the scalp
Supportive measures during this time may include:
-
Zinc supplementation to help reduce excess oil production and inflammatory breakouts
-
Myo-inositol when there are signs of insulin resistance or PCOS-type patterns *(use only when medically appropriate)
-
Reducing dairy and high-glycemic foods, both known to stimulate IGF-1 and acne pathways
-
Regular meals — not extreme fasting, to keep the nervous system and hormones stable
Step 3: Support Detoxification Pathways
This does not mean a detox friend, the body does a great job doing that on its own. However, when hormones fluctuate, how well your body clears them matters. You don’t need harsh detox kits, you need efficiency. Detox pathways include your digestive system and your liver.
Helpful strategies:
-
25–30g fiber daily (vegetables, chia, beans, flax)
-
Daily bowel movements — stagnation can recycle hormone metabolites
-
Hydration paired with cruciferous vegetables (broccoli, cabbage, kale)
-
Reducing environmental hormone disruptors (certain plastics, smoke exposure, excessive alcohol)
Some individuals benefit from a medically guided metabolic reset, especially if symptoms are intense or prolonged.
Step 4: Tend to the Gut and Microbiome
Hormonal changes influence gut health, and gut health influences inflammation, immunity, and skin. PERIOD. You may notice constipation, bloating, or changes in digestion when stopping the pill, these symptoms are not random.
Supporting gut balance may include:
-
Probiotics (especially broad-spectrum or spore-based strains)
-
Prebiotic fibers (onion, garlic, artichoke, asparagus, flax)
-
Identifying food sensitivities with a brief elimination or tracking period
When the gut is supported, the skin often follows.

Step 5: Skin Care That Supports the Change
Systemic change takes time, but topical care can support you during the transition.
Helpful approaches include:
-
Gentle cleansers (avoid aggressive stripping or foaming formulas)
-
Quality moisturizers
-
Sunscreen daily to prevent pigmentation from healing breakouts
-
Topical retinoids, if appropriate, to help prevent clogged pores and help collagen turnover
-
Azelaic acid, Mandelic acid, or benzoyl peroxide depending on skin type and severity
Expect that it may feel a little worse before it improves, the skin often purges while deeper inflammation moves toward resolution.
When It’s Time to Bring in Medical Support
If acne is:
-
Deep
-
Scarring
-
Affecting quality of life
-
Persisting more than 6–12 months
-
Paired with irregular periods or hair changes
Then partnering with a hormone-literate practitioner or dermatologist may be appropriate. Medications like spironolactone, tretinoin, or even isotretinoin may be part of care depending on severity and goals. I love to take a natural holistic approach (which can take time), but everyones preference varies, and something I respect.
Healing Takes Time and That’s Normal
Most women fall into one of these timelines:
Months 0–2: Hormones are recalibrating; breakouts may increase.
Months 3–5: Oil production begins to stabilize; flare-ups lessen.
Months 6–12: Skin often becomes clearer and more balanced as internal systems regulate.
With patience and support, many women find their skin not only returns to baseline, but becomes healthier and more resilient. One of the hardest parts of navigating post-birth control acne isn’t just the physical symptoms it’s the emotional weight that comes with it. Skin sits at the interface of how we present ourselves to the world. Whether we like to admit it or not, acne has the ability to shape how confident, connected, and comfortable we feel in everyday life.
So if you’re going through this, please give yourself grace.
You are not “regressing.”
You are not “doing something wrong.”
You are not alone and you’re not failing because your skin is reacting. Your body is recalibrating.
Hormones don’t "reset" overnight, and neither does the nervous system behind them. Healing real, root-cause healing happens gradually.
It’s okay if you need makeup right now.
It’s okay if you’re avoiding photos for a season.
It’s okay if you don’t feel like yourself yet.
Progress sometimes looks like small shifts before big changes.
Be Mindful of Where You Seek Advice
In the age of social media, everyone has an opinion and skin advice is everywhere. One day, someone is crediting celery juice. The next, it’s slugging with petrolatum. Then it’s dairy-free, gluten-free, seed cycling, spirulina, red-light panels, and a 27-step skincare routine. Some of that information may be harmless or even helpful in context. But some of it can be incomplete, oversimplified, or outright misleading.
Unsolicited advice does not equal medical guidance. And it does not know your hormones, your history, your metabolism, presentation or your personal triggers.
So if you feel overwhelmed by tips, reels, or skin “hacks,” pause. Protect your emotional bandwidth. You do not need to crowdsource your healing. Sometimes boundaries are part of the treatment plan.
Remember: Acne Is a Medical Condition
Forty percent of dermatology intersects with mental health because skin and identity are intertwined more deeply than most people realize.
Breakouts can affect:
-
Self-esteem
-
Social behavior
-
Dating and intimacy
-
Career confidence
-
Mood and anxiety
Research has shown that for many individuals, the emotional distress of acne can feel as significant as the condition itself. Acne is not just cosmetic, it is biological, hormonal, inflammatory, and medical. And your emotional response to it is valid. Shame has no role in treatment.
Know When to Ask for Support
There’s empowerment in trying lifestyle changes, adjusting products, or supporting your gut and hormones, but there is also wisdom in recognizing when professional guidance is needed.
Seek help if:
-
You’re experiencing scarring
-
Breakouts are deep or painful
-
Acne is affecting sleep, confidence, or daily functioning
-
You’ve tried multiple approaches without improvement
-
You feel discouraged or overwhelmed
A trained clinician can help you interpret symptoms, patterns, and labs and build a plan that supports the whole system, not just the surface. There is no prize for struggling through this alone. Needing help doesn’t mean you’re not doing enough, it means you’re ready for a more informed and individualized approach.
With the right supports, skin can transition from drama back to calm, and you’ll likely feel more than clear, more whole.
Reference:
Afzali, H., Ghaffarpasand, F., & Dehghani, M. (2019). Low-dose zinc supplementation for inflammatory acne. Advanced Biomedical Research, 8(36). https://doi.org/10.4103/abr.abr_147_18
Cibula, D., Gompel, A., Mueck, A. O., La Vecchia, C., Hannaford, P. C., Skouby, S., & Dusek, L. (2012). Hormonal contraception and risk of venous thromboembolism. Human Reproduction Update, 18(4), 487–502.
De Pessemier, B., Grine, L., Debaere, M., Maes, M., & Callewaert, C. (2021). Gut–skin axis: Current knowledge of the interrelationship between microbial dysbiosis and skin conditions. Frontiers in Microbiology, 11, 3658.
Facchinetti, F., Orrù, B., & Grandi, G. (2013). Myo-inositol and D-chiro inositol in PCOS: A randomized controlled trial. Gynecological Endocrinology, 29(3), 238–242.
Fabbrocini, G., Annunziata, M. C., D'Arco, V., De Vita, V., Lodi, G., Mauriello, M. C., ... & Monfrecola, G. (2016). Acne diet and gut axis: From clinical research to patient education. Journal of the American Academy of Dermatology, 74(3), 595-598.
Guy, G., & Norman, R. (2022). Androgens and acne: Post-hormonal contraception rebound mechanisms. Journal of Endocrinology and Reproductive Medicine, 15(2), 102–109.
Harper, J. C. (2012). An update on the pathogenesis and management of acne vulgaris. Journal of the American Academy of Dermatology, 66(4), 551–561.
Layton, A. (2020). The use of combined hormonal contraceptives in acne management. British Journal of Dermatology, 183(6), 1097–1108.
Melnik, B. C. (2015). Diet in acne: Further evidence for the role of nutrient signalling in acne pathogenesis. Dermato-Endocrinology, 7(1), e1061388.
Panchaprateep, R., & Tanus, A. (2019). Hormonal acne: Pathogenesis and therapeutic update. International Journal of Women’s Dermatology, 5(5), 316–325.
Smith, R. N., Mann, N. J., Braue, A., Mäkeläinen, H., & Varigos, G. A. (2007). A low-glycemic-load diet improves symptoms in acne vulgaris patients. The American Journal of Clinical Nutrition, 86(1), 107–115.
Sullivan, S. D., Bushnell, D., & Shiff, S. (2020). Post-pill hormone transition timelines. Journal of Women’s Health, 29(5), 612–620.
Thiboutot, D. (2004). Regulation of human sebaceous glands. Journal of Investigative Dermatology Symposium Proceedings, 9(2), 102–105.
Zaenglein, A. L., et al. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology, 74(5), 945–973.
Zimmerman, E., Shinkai, K., & Kimball, A. (2019). The dermatologic implications of hormone regulation via oral contraceptives. Dermatology Clinics, 37(1), 35–45.
